RadCalc adds in-vivo dosimetric verification
The latest release of LAP’s RadCalc QA software majors on customization, intelligent automation and 3D EPID-based functionality for measurement-based patient QA.
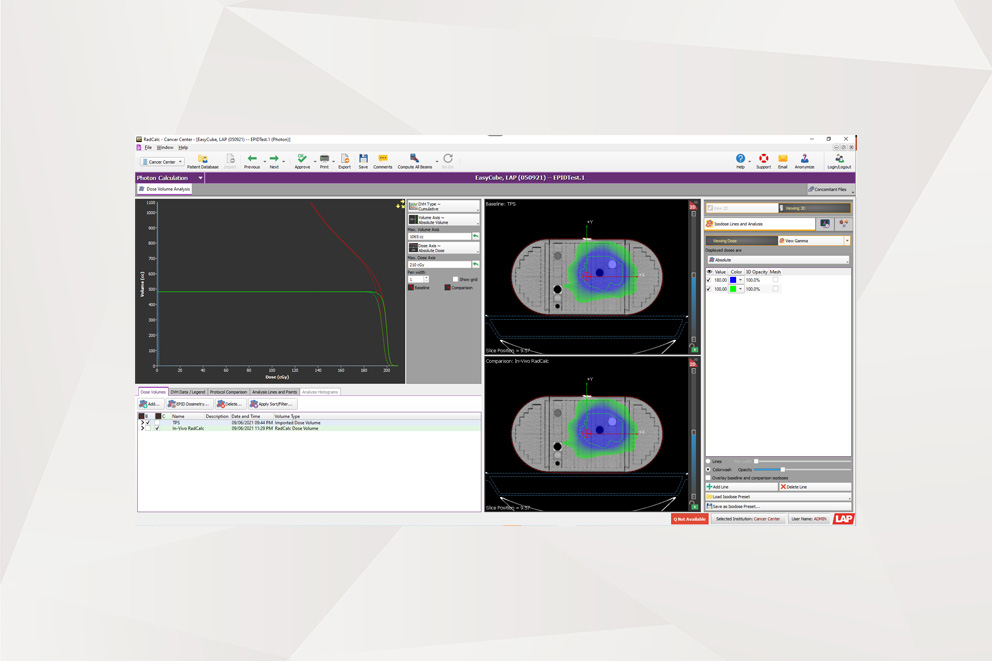
Customer-driven innovation and continuous improvement are once again front-and-centre in the latest release of RadCalc QA secondary check software, a suite of widely deployed quality-assurance (QA) tools that provides medical physicists and dosimetrists with fully automated and independent dosimetric verification of their radiotherapy treatment planning systems (TPS). Top billing in RadCalc v7.2 is the commercial introduction of 3D EPID-based functionality to underpin measurement-based patient QA and in-vivo dosimetric verification. Meanwhile, speed and workflow efficiency remain ongoing priorities for the RadCalc development team following the integration of a range of customization features for intelligent automation into RadCalc AIR, the software’s control centre for automated data import and reporting.
With the release of v7.2, RadCalc’s portfolio of calculations now encompasses secondary dose checks, with the use of point-dose analysis, 3D Monte Carlo or 3D Collapsed-Cone Convolution Superposition algorithms to identify clinically relevant deviations within the entire patient volume; EPID for pre-treatment dosimetry, in which the software reconstructs the dose from the delivered pre-treatment plan on the patient’s original planning CT (giving a direct comparison with both the intended dose from the TPS and RadCalc’s 3D dose second check); and EPID for in-vivo dosimetry to reconstruct the dose delivered during treatment, yielding a direct comparison on the actual delivered dose reconstructed on the original planning CT to evaluate intrafraction changes in the patient.
“We are not aware of any other product on the market able to match RadCalc’s in-vivo 3D capability using EPID-based dosimetry,” claims Craig Laughton, CTO and co-founder of the RadCalc software portfolio, part of LAP’s growing QA product line in radiotherapy. “In the clinic,” he adds, “RadCalc 7.2 enables the medical physics team to compare the whole dose volume versus the original treatment plan, measuring what is actually being delivered in-vivo to the patient during radiation therapy.”
Dynamic systems
Such insights are especially powerful given that patients are dynamic systems, always in flux rather than steady-state. Between treatment sessions, for example, patients can gain and lose weight; their stomach, bladder and bowel contents change; their organs may shift, rotate or deform; and their tumours may shrink, move or rotate.
Those changes can be problematic for traditional radiotherapy regimes that rely on a single CT snapshot of the patient at the start of treatment, with most clinics currently limited in their ability to track geometric deformations in patient anatomy over time. Put another way: a treatment plan attuned to the initial simulation can quickly become suboptimal as radiotherapy progresses over the course of many fractions typically spread across a month or more.
“Our EPID-based module is going to pick up any changes in dose delivery over a course of multiple fractions, triggering a conversation between the clinical physicist and radiation oncologist to understand what’s happening inside the patient,” explains Laughton. “That dialogue could ultimately mean reimaging and replanning of the patient – another important step towards a more personalized approach to radiation therapy.”
“RadCalc 7.2 measures what is actually being delivered in-vivo to the patient during radiation therapy.”
What’s more, RadCalc’s 3D EPID module also has an enabling role to play in supporting the latest hypofractionated and ultrahypofractionated radiotherapy schemes, in which an increased dose per fraction results in significantly fewer overall treatments over a compressed timeframe. The goal, as always, is enhanced targeting accuracy and enhanced dose distribution accuracy – minimizing collateral damage to adjacent organs at risk and critical structures – over a course of treatment running to just one or a few high-dose fractions.
“With a hypofractionated treatment scheme,” notes Laughton, “you need to know if something’s not right straight away – for example, in the case of a machine error or incorrect patient set-up. You can’t afford to wait a week, because in a week the treatment’s done and it’s too late.”
Automate to accumulate
More broadly, intelligent automation remains a long-term fixture on the RadCalc development roadmap, giving medical physicists the power to optimize processes versus their own clinical requirements – customizing which DICOM tags to trigger actions, for example, and new layouts for cleaner workflows. “While we see user-defined automation as a key differentiator,” notes Carlos Bohorquez, RadCalc product manager, “automation is ultimately all about patient safety and minimizing human errors and the burden on clinical resources associated with manual QA tasks.”
According to Bohorquez, the v7.2 release incorporates significant customizations to the RadCalc AIR import and reporting tool to streamline workflows in the clinical environment (e.g. the import/export of clinical protocols; also specific tolerance criteria for each treatment plan based on any DICOM tag the user’s TPS is able to export). “It’s an ever-evolving process to provide clinicians with true and faithful automation for existing and emerging radiotherapy technologies,” he explains.
“Automation is ultimately all about patient safety and minimizing human errors.”
That’s certainly true for RadCalc’s new 3D EPID module, which imports the necessary EPID data/image files for processing before sending to the Collapsed-Cone dose engine to calculate the dose. “The EPID-based solution needs further automation so that the physics team can use it on a routine off-line adaptive basis, eliminating manual interventions within the RadCalc UI,” explains Bohorquez. “That work will be the focus of our next release in a few months’ time, increasing the clinical and operational impact of this functionality.”
Another priority for the RadCalc development team is to tap into the scripting features of leading TPS offerings. “In effect,” Bohorquez concludes, “these are changes that we will implement outside of RadCalc to make the software’s automation tools even more powerful to the end-user in the clinic.”
Find the original article on the Physics World website.